Have you, or has someone you care about, recently sustained a head injury or a concussion? Or maybe you suffered a concussion and are on the road to recovery but still don't feel like you are "yourself" again. Perhaps you found this article because you want to understand what is happening to you. Or maybe you're searching for answers to get past the brain injury and symptoms you're experiencing and return to life as it was before. You're not alone. Best estimates suggest that approximately 1 in 10 people will sustain a concussion in any particular year. Due to a lack of public education causing underreporting, a precise definition, standard of care, and inadequate data collection, the number of concussions that occur each year may never be discovered.
Concussions confuse everyone, including doctors and researchers, for many reasons. There is very little formal training/ medical education on concussions. In the research, over 30 "official" definitions of concussions are established, all with different diagnostic criteria. Alone, this makes establishing a concussion diagnosis difficult. Additionally, a head injury is not always a concussion. All concussions are considered mild traumatic brain injuries, but not all mild traumatic brain injuries are considered concussions. And research suggests that as few as 23% of concussions will make a full recovery, based on the resolution of symptoms. The rest of those concussed may persist to post-concussion syndrome, lasting from 3 months to years (sometimes considered permanent). Confused yet? Everyone else is.
Before 2023, a concussion was reserved for mild traumatic brain injuries sustained while participating in a sport. The American College of Rehabilitation Medicine (one of the original groups of lexicographers of the definition of concussion/mTBI back in 1993), now being led by Dr. Noah Silverberg of the University of British Columbia and Dr. Grant Iverson of Harvard University, has clarified the diagnosis of TBI, mTBI, concussion, and introduced the term "suspected mTBI". Dr. Antonucci recorded a 30-minute video to explain the definition and criteria fully.
It is important to note that all concussions are mTBIs, and all mTBIs are (clearly) TBIs, but the opposite is not true. Therefore, we need to know the criteria that will allow us to diagnose the form of brain injury someone has sustained accurately.
The "mild" TBI qualifier can be applied when none of the following have been met
A "concussion" is an mTBI (meeting the criteria above) in which imaging was either negative or was not warranted.
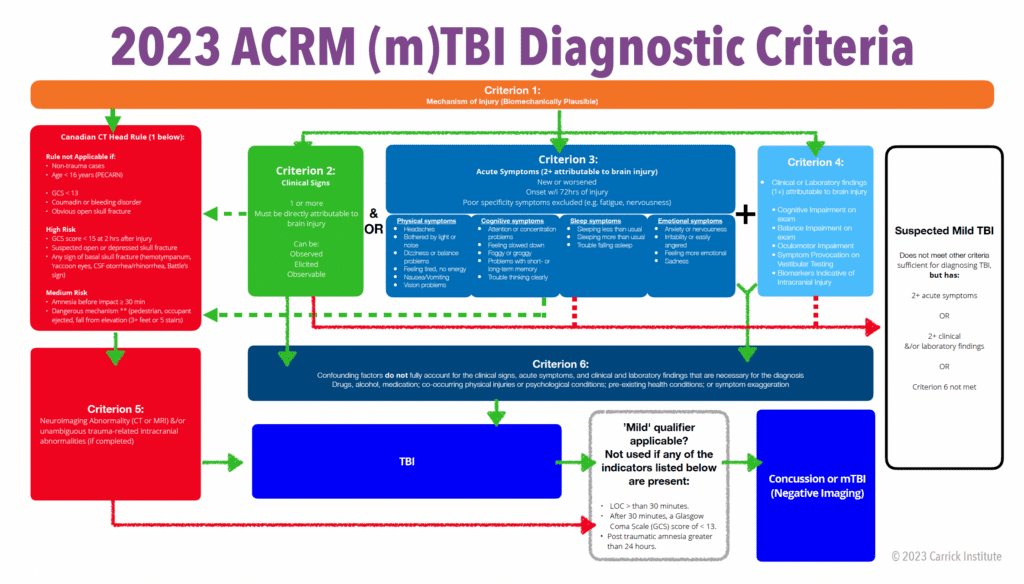
A "suspected mTBI" should only be diagnosed when an individual has a presentation after a biomechanically plausible mechanism of injury that does not fully meet the criteria of a concussion or mTBI.
In 2014, Dr. Chris Giza published a seminal paper describing, in detail, a concussion's complex and system effects. A concussion is caused by a rapid change in the velocity of the head (from still to moving or moving to still). That quick change in speed causes stretching of brain tissue, similar to when you sprain a ligament or strain a muscle. That stretching causes damage to nerve cells which disrupts signaling, causing them to "short circuit" and become active when they're not supposed to be. This is why some people "see stars" or get their "bell rung"; because the brain area responsible for seeing or hearing (respectively) is injured. At the same time, blood vessels that deliver energy-sustaining oxygen and sugar are also stretched and sometimes even torn. This causes decreased blood flow and fuel to the same over-excited areas. This decoupling of fuel and energy causes brain cells to die. The injured brain cells release chemicals that cause inflammation, which causes swelling (causing someone to experience nausea, vomiting, and headache- possibly necessitating medical attention and treatment). This process triggers a healing response that removes dead brain cells and causes injured cells to hibernate. This all occurs within the first 48 hours. The brain naturally begins to re-organize during that time based on the demand. This remodeling process (plasticity) is not good in this scenario. This is why it is imperative to rest until this process has ended (less than 72 hours). The injury of brain tissue, combined with the reorganization of brain function, causes short- and long-term concussion symptoms. It needs to be addressed in any concussion treatment for successful concussion recovery.
Always play it safe. If someone hits their head, immediately get that person to a safe and quiet place where they can be evaluated by someone trained in concussion management. The first priority is to prevent repeated concussions. If they are an athlete playing a contact sport and sustained a sports concussion, this might be a coach or an athletic trainer. If it is not a sports-related mTBI, it may be a sports medicine/family medicine doctor, a physical therapist, chiropractor, EMT, or other health care provider. If, for some reason, nobody around is trained in managing concussions, talk to the person and observe their behavior. Here is a sample conversation that you might have.
Your job is to listen and observe. Do they sound calm, collected, clear-headed, and oriented? Are they slurring their words? They should receive medical attention and a concussion evaluation immediately if anything seems abnormal. Failure to receive proper treatment, or a second concussion that occurs before an initial concussion has not healed, can cause permanent brain damage.
A concussion will always have two or more symptoms that begin within 72 hours of injury. Suppose you or someone you know sustained a head trauma or trauma that caused their head to shake violently. In that case, it should be assumed that they have a concussion unless proven otherwise by a healthcare provider trained in concussion. Symptoms may appear at the time of injury or sometimes as late as 3 days after. The most common symptom is a headache, but there are more than 50 symptoms that someone with a concussion might experience. These symptoms may include including feeling frustrated or impatient, anxious, sad, irritable, more emotional, restlessness, sweats/chills, hot/cold extremities, pressure in the head, worse symptoms after physical exertion, nausea, light headed/ uncomfortable standing, bladder discomfort/changes, irregular/rapid heart rate, trouble with memory, difficulty concentrating, slower speed of thinking, confusion, trouble word/name finding, feeling in a fog, not feeling right, fatigue/low energy, trouble falling or staying asleep, not feeling rested, sleeping too much, needing more sleep, muscle weakness, numbness or tingling, sensitivity to noise, back pain, headaches, muscle pain/aches, eye pain, skin/muscle twitching, balance problems, neck pain (stiffness), dizziness, sensitivity to light, blurry/double vision, difficulty with moving scenery, motion intolerance, visual disturbance (snow, spots), eye strain, and more. The reality is that your brain is the organ that dictates your perception and function. If the brain is injured, any element of our life could be affected.
Once a healthcare provider determines that you or someone has sustained a concussion, there are many fallacies about what to do next. Some of them are blatantly wrong, like "head injuries are part of life/part of the game," and they aren't anything to worry about. Others are more of a misunderstanding of the facts, like "do not let the person go to sleep at night." Or "lock them in a dark room and do not engage in any activities until they are better."
Here's the truth. Concussions, like any injury, need time to heal before returning to normal activity. The critical time for rest is the first 48-72 hours. During that period, get plenty of sleep (it's perfectly fine to check in on the person to make sure they're breathing properly and they are resting peacefully- but don't wake them up), physical rest (refrain from anything more than mild physical activity), cognitive rest (refrain from any intense mental activity), and avoid any situation where a second concussion might occur. Take time off from work/school. It's essential to be extra cautious because natural healing processes are happening during that time, and sustaining another injury could be catastrophic. Contact a primary care doctor and schedule a follow-up appointment. Consult with a doctor to see if over-the-counter medications could be taken to help with symptoms. Often taking Asprin or NSAIDs (ibuprofen, naproxen, etc.) will be discouraged because they mask symptoms and thin the blood, which may increase the risk of bleeding the injury. Tylenol is most recommended for pain, and other over-the-counter medications for symptoms.
It's always better to err on the side of safety. Unless someone trained in concussion evaluation has advised that a hospital visit is unnecessary, it is always safe. Not many people have regretted going to the emergency room and being told: "everything is alright." If you are not able to be evaluated, here are some things to consider
Imaging is only warranted under particular conditions (typically over the age of 60, severe headache, unmanageable neck pain or instability, suspected skull fracture, deteriorating neurological signs, or multiple episodes of vomiting), in which case a non-contrast CT scan of your brain will often be ordered. If at least one of the Canadian CT Head Rules conditions is not met, a brain scan is likely unnecessary. MRIs are rarely helpful in the diagnosis or management of concussions. You should not return to regular activity until a second concussion evaluation is performed, the testing has normalized (you may still have symptoms), and you have been "cleared" to return to your normal activities by a licensed and trained healthcare provider. Returning to sports or activities too soon and sustaining another concussion may result in a more severe concussion or second impact syndrome, which can have deadly consequences.
Your body is miraculous at healing itself. However, healing does not always equate to "getting back to normal." For example, your body will heal if you get cut, but a scar will remain. If you roll your ankle, it will heal. Still, that ankle will be more susceptible to future injuries if it is not rehabilitated. The same is true for brain injuries. Research suggests that for a first concussion, the symptoms will resolve in approximately ten days for adults and 14 days for children (typically 50% longer for multiple concussions). This is true in many circumstances, but in many cases (10-77%), symptoms will persist for months or years, which was called "post-concussion syndrome, but is not being referred to as "persisting post-concussion symptoms." Research has also found fewer cases resolve without treatment when looking at brain function instead of symptoms. This is even true for "mild" concussions. Additionally, there is some support that repetitive sub-concussive injuries may lead to chronic traumatic encephalopathy (or CTE).
Commonly, after 10-14 days have passed, and a patient is not feeling back to normal again, a primary care provider will refer the patient to a concussion specialist. These specialists are often neurologists, physical therapists, chiropractors, neuropsychologists, athletic trainers, occupational therapists, neuro-optometrists, or other disciplines trained in concussion management.
Additionally, the relationship between head injury and neck injury is often overlooked. The mechanism of injury that causes a concussion may also injure the neck, especially in women. Therefore, an evaluation by a chiropractor or a sports medicine physician is essential to resolving concussion symptoms (particularly neck pain).
When it comes to concussion treatment or concussion treatments, there is no "one size fits all" treatment. Brain injuries are as unique as one's brain; therefore, a concussion program for a brain injury must also be as unique as each brain.
Doctors use two main methods to determine what type of concussion therapy will be prescribed: symptom-based or function-based approaches.
The 50± concussion symptoms were once divided into three types: physical symptoms, cognitive symptoms, and emotional symptoms. More recently, these symptoms have been further categorized into categories. These categories are called concussion subtypes (or phenotypes). We will expand upon these phenotypes in other articles.
There are also 2 "associated categories" that often occur secondary to the subtypes above:
By assessing your symptoms and assigning them to their proper phenotype, a doctor can choose to manage your concussion symptoms with medications or refer you to a concussion clinic for a specific type of symptom-based concussion therapy.
Symptom-based management is a traditional method of treating concussions (and many other conditions). In this style, care is directed at eliminating symptoms with a "cookie cutter" approach, with little consideration for brain function. This type of treatment typically involves medications or therapies to reduce symptoms affecting the individual with the concussion. Drugs and some therapies are very effective at reducing symptoms but often come with undesirable side effects, do not address underlying brain dysfunction from the injury, and sometimes have rebound effects (symptoms worsen when therapy is discontinued).

The symptom-based approach is like a game of "whack-a-mole." It is reactive (chasing symptoms) instead of proactive (fixing function). Usually, both the doctor and the patient end up frustrated.
While people often feel better with the symptoms-based approach, the FDA has not approved any drugs to treat concussions. No evidence supports that medications or drugs effectively resolve or shorten a concussion's duration.
The second approach to concussion treatment is function-based management. This type of management uses a systematic approach to collect health information (history, etc.), concussion symptoms and measure brain health through particular types of testing. The provider will then examine the function of each subtype, compare your values to normative data, and identify what functions/areas have sustained an injury and need rehabilitation. This method allows the provider to uncover the root cause of your symptoms, often employed by functional neurologists trained explicitly in concussion care.
The function-based approach to concussion is central to functional neurology (See "What is Functional Neurology"). This approach looks at the brain's functional integrity through sophisticated testing, advanced imaging, and/or a thorough physical examination. The data collected from these evaluations are then interpreted, considered against your concerns and goals, and compared against solid scientific research to create unique treatment plans that help rehabilitate the brain through neural plasticity (See "What is plasticity?"). While there is not a lot of research supporting the efficacy of these programs, there is support for their safety. With everything in life, when making a decision, you should always consider potential risks to potential benefits.
A primary cause of concussion symptoms and post-concussive syndrome is remodeling brain function and inflammation. These changes occur due to genetics, plasticity, or the brain's remodeling to injury. Functional neurology attempts to identify decompensated functions (not functioning normally) and create a treatment program to restore their function, once again, through plasticity. By prescribing specific sensory, motor, and cognitive exercises, a functional neurologist or a provider trained at the Carrick Institute and certified by the American College of Functional Neurology can re-wire the brain after an injury. They employ therapies that include vision therapy, physical therapy, occupational therapy, speech therapy, sports medicine, physical rehabilitation, chiropractic, vestibular therapy, mental health coaching, balance training, cardiovascular conditioning, cognitive rehabilitation, coordination training, sensory-motor processing drills, QEEG-guided neurofeedback, hyperbaric oxygen therapy (HBOT), photobiomodulation, nerve stimulation, and other modalities. Remember, the most important treatments are the ones that are appropriate for the individual concussion, and that's impossible to determine without a formal consultation and a comprehensive evaluation.
Ensuring that a person follows a physician-guided returning to activities (RTA) or returning to play (RTP) protocol after a concussion is critical to prevent permanent damage. Ideally, every person in the world would have a Brain Health Assessment before sustaining a concussion. If so, the healthcare provider could measure precisely when the person's brain has healed and when they can resume normal activities/contact sports. However, many people are not proactive about their brain health, so that's not usually the case. A concussion doctor tries to aim without a target when they do not have data from a pre-injury baseline test. We look at symptoms, assessments, performance, and tolerance to increased demand to determine when a patient has returned to "normal." The challenge is that your normal may differ from someone else's. We allow patients to return to full activities and sports once we have established that you have achieved their normal pre-concussion status.
Please share this article on your social outlets. Understanding concussions and how they can be treated may change someone's life or give hope to someone who may feel like they've run out of options.
