Plasticity is used in brain science to describe the brain's ability to change and adapt throughout an individual's lifetime in response to various environmental, cognitive, and developmental factors. This phenomenon is fundamental for the development of new skills, the formation of memories, and the recovery from injuries or diseases that affect brain function. Brain plasticity is based on the ability of neurons to modify their relationship, or connections, with other neurons in response to changes in neural activity. This process, known as synaptic plasticity, allows the brain to reorganize its networks and optimize its function in response to different events and challenges.
One of the most important forms of synaptic plasticity is long-term potentiation (LTP), which occurs when a synapse's repeated activation or stress strengthens the synaptic transmission, or connection, between the pre-and post-synaptic neurons. This process, the cellular basis of learning and memory, allows the brain to continuously remodel, adapt, and change how it interacts with the environment.
Another form of plasticity is neurogenesis, which refers to generating new neurons in the brain. This process is thought to occur primarily in two regions of the brain: the hippocampus, which is involved in learning and memory, and the olfactory bulb, which is involved in the sense of smell. Neurogenesis is thought to play a role in the adaptation of the brain to new experiences and the repair of brain damage.
The importance of plasticity lies in its implications for human health, well-being, and disease. Plasticity allows individuals to learn new skills, adapt to changing environments, and recover from injuries or diseases that affect brain function. For example, brain injury patients can benefit from neuroplasticity-based rehabilitation programs that help them relearn lost motor skills and improve their cognitive function.
Sensory experiences are the most important factors in creating plasticity. When an individual is exposed to multiple new sensory experiences or a singular impactful or stressful experience, the brain modifies its neural networks to optimize its functioning in response to these demands. This is known as experience-dependent plasticity, and it occurs throughout the lifespan. For example, learning a new skill, a first kiss, or a tragedy can lead to changes in the brain that facilitate remembering and repeating these experiences.
Another factor that contributes to plasticity is injury or neurological disease. When the brain is damaged by injury or disease, it can respond by reorganizing its neural networks to compensate for the damage. This is thought to be one of the primary mechanisms by which concussions may sometimes resolve on their own. This type of plasticity is known as "compensatory plasticity." It is the target and basis of many rehabilitation programs that aim to improve brain function after injury or disease. This is why concussion patients may benefit from rehabilitation programs that help them relearn sensory-motor processing skills by promoting compensatory plasticity.
Genetics also plays a role in brain plasticity. Some individuals may have a genetic predisposition to greater plasticity, allowing them to learn new skills more easily or recover quickly from brain injuries or diseases. Additionally, certain genes are involved in the regulation of synaptic plasticity and neurogenesis, which are two key mechanisms of plasticity in the brain regulating synaptic plasticity and neurogenesis,
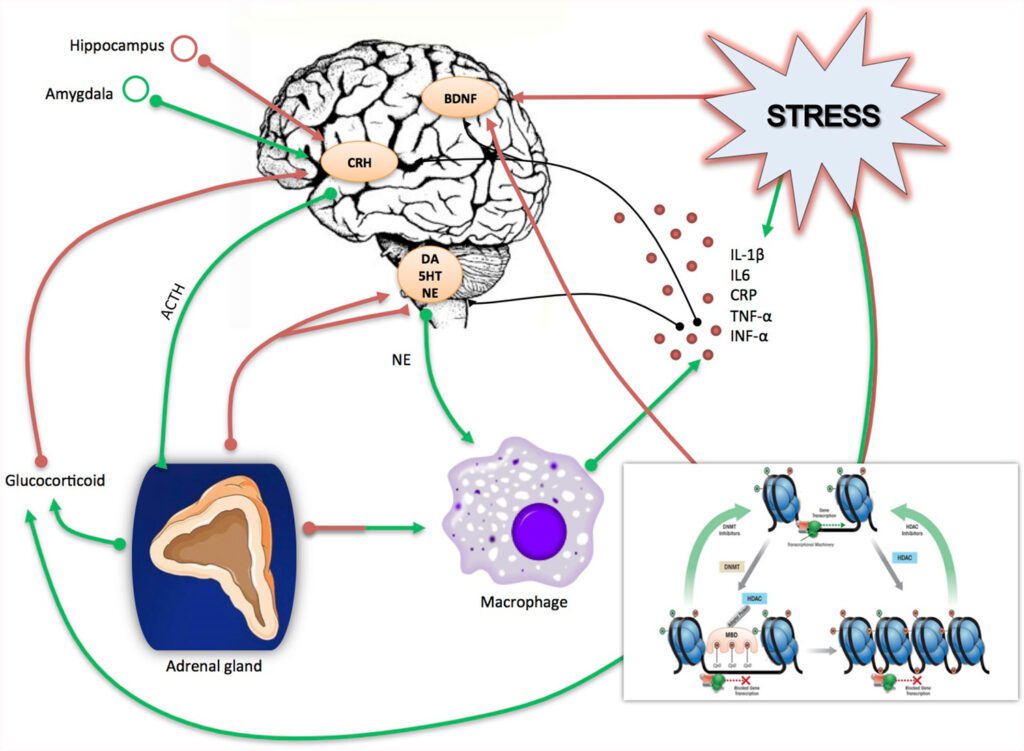
Finally, several neurotransmitters and signaling molecules play important roles in neuroplasticity, which refers to the brain's ability to change and adapt in response to experience.
Some of the major neurotransmitters involved in neuroplasticity include:
In addition to neurotransmitters, several other types of signaling molecules play important roles in neuroplasticity, which refers to the brain's ability to change and adapt in response to experience. Some of the major signaling molecules involved in neuroplasticity include:
Overall, these signaling molecules work together to modulate plasticity in the brain. Their effects depend on the specific brain regions and circuits involved, as well as the timing and intensity of their release.
While brain plasticity is generally considered a positive trait that allows the brain to change and adapt throughout an individual's lifetime, not all forms of plasticity are good. In some cases, plasticity can be maladaptive and contribute to the development or persistence of neurological and psychiatric disorders.
One example of maladaptive plasticity, or plastic deformation, is the overgrowth of neural networks that occurs in some forms of epilepsy. In these cases, excessive synaptic connections can lead to seizures and other disorder symptoms. Similarly, plasticity can sensitize neural pathways in chronic pain conditions, increasing pain sensitivity and decreasing pain tolerance. Plasticity can lead to the sensitization of neural pathways in chronic pain conditions.
Other examples of maladaptive plasticity are the reorganization of neural networks that occurs in concussions, long-standing vestibular disorders, and even long-duration space flight where the brain has maladapted to micro-gravity and hypo-magnetism. While compensatory plasticity can help individuals regain lost function after these injuries, in some cases, maladaptive plasticity can lead to changes in neural connectivity that contribute to persistent sensory, cognitive, or motor deficits. Maladaptive plasticity can alter the way that an individual perceives themselves, the world that they exist, the way they think, their personality, and even subconscious functions (like their blood pressure, heart rate/rhythm, hormones, etc)
In addition, plasticity can be influenced by environmental factors or harmful or stressful experiences, such as exposure to chronic stress, trauma, or substance abuse. These experiences can lead to maladaptive changes in neural networks that contribute to developing mood and anxiety disorders, addiction, and other mental health conditions. For example, in post-traumatic stress disorder (PTSD), the reactivation and consolidation of traumatic memories can contribute to the persistence of the disorder.
Similarly, plasticity can also lead to strong associations between drug use and environmental cues, making it difficult to break the cycle of addiction.
Harnessing plasticity, or the brain's ability to change and adapt, can be a powerful tool for improving health and performance. By understanding plasticity mechanisms, researchers and clinicians can develop interventions promoting adaptive brain changes.
One way to harness plasticity for health and performance is through targeted training programs. Most training programs have a common, fundamental framework involving sensory-motor integration. If you think of the brain as a computer system, like a computer, it needs input to function (like a mouse or keyboard). The inputs for the brain are senses (olfaction, vision, audition, gustation, proprioception, and the one that everyone overlooks— vestibuloception). Each sense is fundamentally linked with a motor function to approach a stimulus or withdrawal from it. This is the basis of sensory-motor training. Once a person is introduced to a sensory stimulus and responds with a motor function, they sense their response and refine it to be either more efficient or more appropriate. This is called coordination and cognition. This is how athletes can benefit from training programs that employ sensory-motor drills to target specific neural networks involved in their sport, such as motor coordination or spatial awareness.
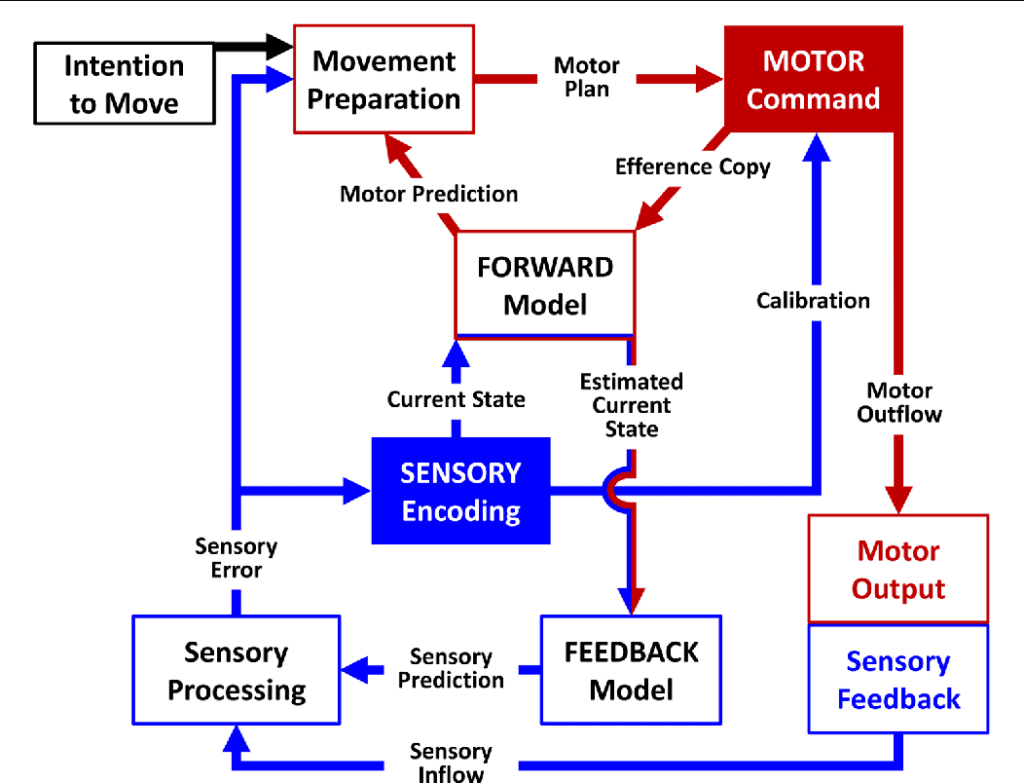
If sensory information is erroneous, the brain's sensory encoding is inaccurate and will create an inappropriate motor function. Think about this as "poor quality in yields poor quality out." Since sensory information is the foundation of motor function and cognition, correcting aberrancies in sensory processing is fundamental for most rehabilitation programs.
Another way to harness plasticity is through the use of device-generated brain stimulation techniques. Transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) are two of many non-invasive techniques that can modulate neural activity and promote plasticity in different brain regions. TMS can be used to stimulate specific regions of the brain, while tDCS can be used to enhance or suppress neural activity in targeted networks.
In addition, plasticity can be harnessed for all nervous system areas, including neurological and psychiatric disorders. For example, stroke patients can benefit from rehabilitation programs that promote compensatory plasticity to help them regain lost motor skills. Similarly, individuals with depression can benefit from cognitive-behavioral therapy, which promotes adaptive changes in neural networks involved in emotion regulation.
Furthermore, plasticity can also be harnessed for cognitive enhancement. For example, brain training games and other cognitive training programs can promote plasticity in the prefrontal cortex, which is involved in executive function and working memory. Additionally, mindfulness meditation has been shown to promote plasticity in the hippocampus, which is involved in learning and memory.
Jeffrey Kleim, Ph.D., a neuroscientist and expert on neural plasticity, has proposed 10 principles for applying the concept of plasticity to improve brain function. These principles guide designing interventions that promote neuron-to-neuron communication and adaptive changes in the brain.
Applying the ten principles of plasticity proposed by Jeffrey Kleim can guide the development of interventions that promote adaptive changes in the brain. These principles highlight the importance of specific and challenging training programs, the timing and intensity of interventions, and the emotional salience of tasks. Understanding plasticity mechanisms and designing interventions that harness their power can improve brain function and promote lifelong learning and growth.

Dr. Antonucci has spent the past decade learning and developing different ways to harness these ten principles of plasticity to help individuals with persisting concussion symptoms. The result is his immersive treatment program, which has helped thousands of patients live their best lives.
A great deal of thought has gone into creating our "Immersive Program," which is a 5-day program "inpatient-like" program. For this program, people travel to my facility, stay in a nearby hotel or house, and dedicate 100% of their week to making transformational changes in brain function and disconnecting from the stressors of home, work, school, and the rest of life ("Salience Matters"). This style of care also helps us manage the "Interference Matters" principle. Over these five days, I will construct a customized rehabilitation program based on an extensive evaluation. In a 3-hour evaluation, I comprehensively measure an individual's sensory-cognitive-motor system to identify any maladaptive plasticity using established and novel evaluation procedures. Once we have identified functions that need modification, I create an intervention program that specifically targets the tasks and networks that need to change ("Specificity Matters"). This involves doing something ("Use and Improve It") and NOT doing something ("Use it or Lose it") to reshape the targeted neurological networks. Patients are treated for two to three 60 to 90-minute, multi-modal daily sessions involving proprioception, vision/oculomotor, vestibular, coordination, and cognitive therapies, harnessing the "Transference Matters" principle. This schedule also allows us to build on the "Intensity Matters" and "Repetition Matters" principles.
Some principles or variables, such as age and timing, are more difficult to control and manipulate in a treatment program. We would love to see patients early in their injury and/or when they are young, but that isn't always possible. Despite not all of our patients being young or having "fresh" injuries, we have been fortunate to create life-changing transformations for most of them. Our results have been published in over 60 peer-reviewed medical publications, many of which can be found here: Dr. Antonucci's Publications on Loop: The Open Science Research Network
